Position statement
Sport-related concussion and bodychecking in children and youth: Evaluation, management, and policy implications
Posted: Jan 18, 2023
Principal author(s)
Kristian Goulet MD FRCPC, Suzanne Beno MD FRCPC; Canadian Paediatric Society, Injury Prevention Committee
Paediatr Child Health 2023 28(4):252–258. 
Abstract
Concussions are a common injury both within and outside sport and recreational settings, and they remain a serious concern for children and youth. Any young person suspected of sustaining a concussion should be medically evaluated as soon as possible, and when the injury occurs during sport, the individual must be removed from play immediately to avoid secondary injury. A brief initial period of physical and cognitive rest is followed by supervised, stepwise return-to-learn and return-to-play protocols. All individuals involved in child and youth sports and recreation must be able to recognize risk for, and signs and symptoms of, concussion. They must also ensure that any participant suspected of sustaining a concussion is properly evaluated and managed by qualified medical personnel. Evolving data and literature have strengthened both our pathophysiological understanding of concussion and guidance for clinical management, especially related to acute care, persistent symptoms, and prevention. This statement also re-examines the relationship between bodychecking in hockey and injury rates, and advocates for a change in policy in youth hockey.
Keywords: Adolescents; Bodychecking; Children; Concussion; Return to learn; Return to play; Sport; Youth
Concussions, also known as mild traumatic brain injuries (mTBIs), remain a prevalent and important cause of global morbidity in children and youth. Traumatic brain injury is the leading cause of paediatric trauma death and disability worldwide, with concussions comprising 80% to 90% of all TBIs [1]. An estimated 200,000 concussions occur annually in Canada, with children and youth affected primarily [2][3]. The field of concussion diagnosis and management is evolving rapidly, with significant global engagement [4]. The Canadian Paediatric Society (CPS) published a statement on sport-related concussion in children and youth in 2012 [5]. Major advancements in our understanding of concussions since have necessitated a revision to capture these developments, with additional focus on the role of bodychecking in hockey-related concussion epidemiology. The statement summarizes and highlights recent evidence and current best practice guidelines for managing concussion in children and youth.
Diagnosis and assessment
Any child or youth experiencing a significant fall or hit should be assessed for head injury and possible concussion. The 5th International Consensus Statement on Concussion in Sport defines sport-related concussion (SRC) as a TBI induced by biomechanical forces resulting in rapid onset of short-lived impairment of neurological function that resolves spontaneously [6]. A concussion may result from a direct impact to the head, neck, face, or elsewhere on the body that transmits an impulsive force to the brain. Concussions represent a primarily functional rather than a structural brain injury, and no abnormality is seen on standard structural neuroimaging studies. SRCs can cause a range of clinical signs and symptoms. Resolution typically follows a sequential course, with the vast majority of concussions resolving within 4 weeks, without long term complications. However, symptoms can also be more prolonged. The diagnosis of an acute SRC involves a range of domains, with concussive signs and symptoms including (but not limited to) physical manifestations, cognitive impairment, neurobehavioural features, and sleep/wake disturbances (Figure 1).
Figure 1. Clinical signs and symptoms of concussion
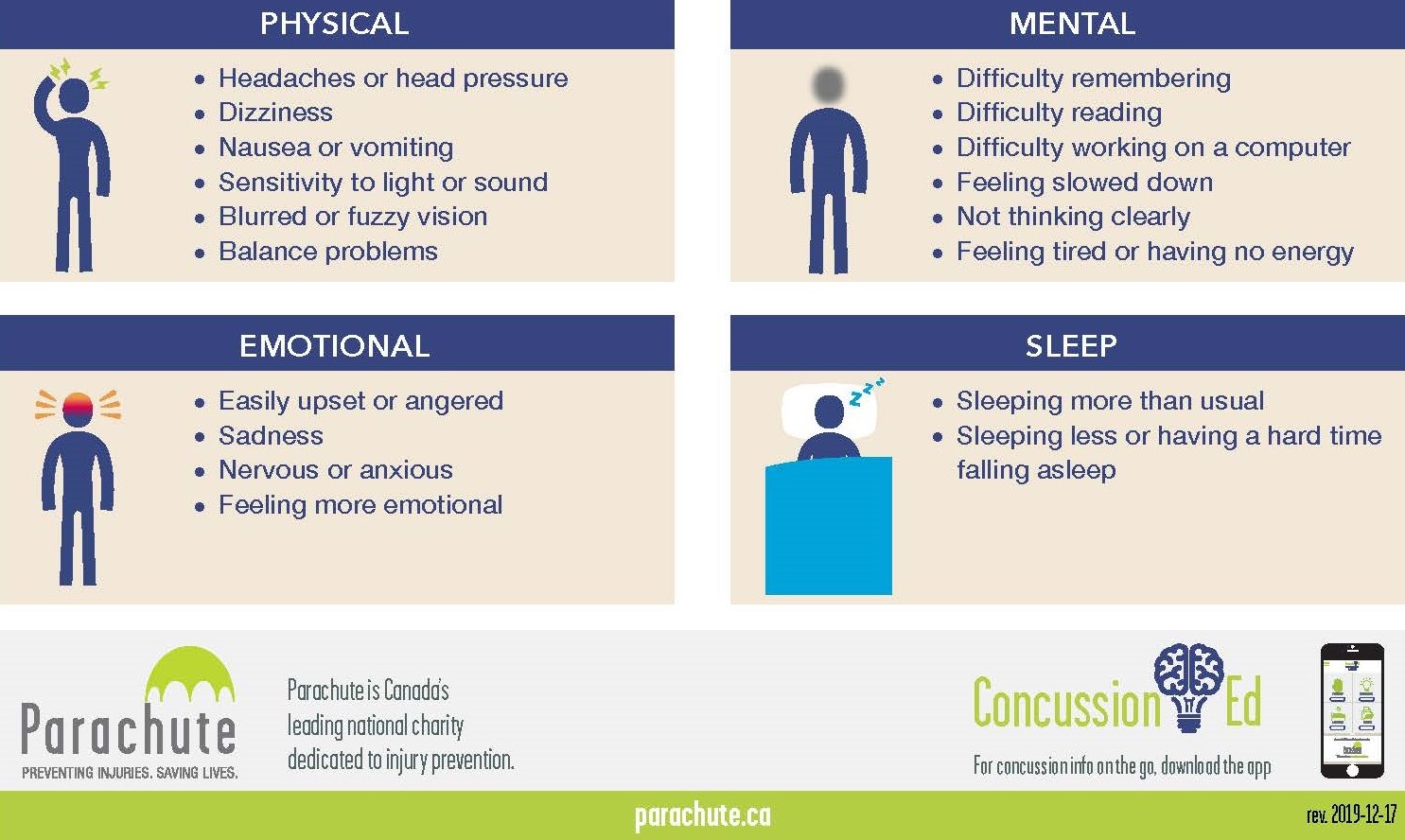
Source: Parachute. Reproduced with permission
After trauma, it is imperative to ensure patient stability and assess for other injuries, specifically structural head trauma and injury to the cervical spine. Reducing environmental stimulation can allow for more complete and accurate evaluation. When managing concussions, health care providers (HCPs) should be aware that most concussions do not involve a loss of consciousness or focal neurologic findings, and symptoms may present hours to days after the injury [6][7]. Also, many conditions can mimic concussion symptoms. Clinical signs or symptoms related to concussion should: 1) include any of those listed in Figure 1) begin after the head injury; and 3) should not be readily explained by a co-occurring condition. Consideration should be given to possible alternative diagnoses (e.g., structural head injury) and confounding variables (i.e., pre-existing comorbid or extracranial factors) before establishing a concussion diagnosis [8].
Diagnostic tools
Because many variables can influence symptomatology, no single test or assessment tool can immediately diagnose a concussion or be used to accurately predict how a child will recover from any one head injury [6][7][9]. The Child SCAT5, which is used for children 5 to 12 years of age, is widely considered to be the best available assessment tool to assist in diagnosing SRC. Child SCAT5 includes red flags, observable signs, the Glasgow Coma Scale, cervical spine assessment, background, child and parent reports on symptoms and memory assessment, cognitive screening, and neurological screening, including balance examination [10]. For persons older than 13 years, the SCAT5 can be used. HCPs should take a multifaceted and age-specific approach to children and youth with suspected concussion, even when they do not exhibit symptoms initially. Ideally, serial assessments involve administering validated symptom rating scales and evaluating balance and cognitive function [8].
Technological advances under study for concussion assessment but not yet in mainstream use include neuroimaging, brain biomarkers, computerized testing, and head impact sensors. Certain advanced neuroimaging modalities hold promise but are not used for diagnosis at the present time [2][4][6][11]. Similarly, multiple brain biomarkers, with s100b of specific interest, have not demonstrated reliable evidence for regular use in concussion management [12]. EEGs and genetic testing are also being studied but have not been endorsed [1][4][6]. Helmet sensors, despite their promise and widespread use, are not yet validated and may contribute to inaccurate representation of head injury [6]. While formal neuropsychological testing is considered an important tool in the multimodal assessment and management of concussion, neurocognitive tests should not be used or relied upon by themselves for diagnosis, and baseline testing has not been established as a standard of care for many reasons, including poor sensitivity and reproducibility [6][8][13][14].
Persistent symptoms
While most children and youth with a concussion recover within 4 weeks [8][15], they can also experience more prolonged symptoms. Recent research has identified risk factors that contribute to prolonging symptoms and slowing recovery. One predictive tool for use in the emergency department can be found at www.5pconcussion.com/en/scorecalculator [16]. Key risk factors were identified in a comprehensive meta-analysis published in 2017: concurrent or past mental health issue, concurrent cervical injury, elevated initial symptom burden, age <18 years (with highest risk at 13 to 17 years of age), female sex, and the presence of ocular dysfunction [17]. The Centers for Disease Control and Prevention (CDC) has also identified premorbid history of mTBI, previous neurological or psychiatric disorder, learning difficulty, pre-injury “post-concussive” symptoms, and family and social stressors as further risk factors for persistent symptomatology [4].
In cases where symptoms persist for >3 months, factors other than head injury and resultant neuronal damage should be considered as primary drivers of symptomology [8][17]-[19]. Prolonged cognitive deficits following a concussion are now believed to be more attributable to depression, anxiety, sleep problems, or unrecognized attention disorders than to the injury itself, which has significant implications for treatment [8][17]. To accurately delineate the etiology of symptoms, the CDC is advocating for a formal neuropsychological evaluation in paediatric patients. For families who cannot access this type of testing, a referral should be made to a physician or nurse practitioner with experience treating patients living with prolonged symptoms. Identifying and addressing confounding variables are crucial to optimize function and well-being in children and youth with lingering concussion-related symptoms.
Studies have shown, for example, that when patients misattribute their symptoms to head injury, it negatively impacts recovery, a phenomenon termed “expectation as etiology” [20]-[23]. The early identification of mental health disorders, and of young people at particular risk for any reason, is essential to prevent exacerbation of mental health problems during the recovery period [7]. The term ‘post concussion syndrome’ has passed out of use because concussion-related symptoms are no longer considered “syndromic” in nature, but rather as reflecting many pathologies. ‘Persistent post-concussion symptoms’ (or PPCS) is the current and most widely accepted term [18].
Treatment of concussion and persistent post-concussion symptoms (PPCS)
To access a detailed, comprehensive review of concussion management, see the Living Guideline for Diagnosing and Managing Pediatric Concussion. This guideline distinguishes among acute head injury, concussion, and PPCS based on the broad range of etiologies and clinical presentations that may be in play. This statement focuses on stepwise management, with specific focus on education, rest, return to learn, and return to play.
Education
Timely, appropriate, and specific education on concussion management is essential. HCPs should reassure children, youth, and families that the vast majority (70% to 80%) of young people with concussion recover without significant difficulty within 4 weeks [4]. Education should focus on a progressive, sequential trajectory of care, warning signs that may suggest more serious injury, and how to prevent further injury based on adherence to return-to-learn and return-to-play protocols.
Rest
A significant change in concussion management in recent years involves the role of rest. Prolonged rest is now recognized as having a potential negative effect on recovery, while low-impact exercise can be beneficial [24]. An initial 24 to 48 h of restrictive rest is still recommended, followed by a gradual increase in physical and cognitive activity [7], but initiating light exercise at 72 h has been shown to be safe and associated with fewer symptoms at 2 weeks post-injury [25]. Throughout management, the child or youth should maintain a level of activity that does not worsen or produce new symptoms or put them at risk of re-injury. Social activities can increase progressively at the same time [4][7]. The process of recovery should follow a stepwise approach until the individual is participating fully in routine physical and cognitive activities [4][6].
The process of returning to school symptom-free should be completed before returning fully to sport participation, especially when risk for impact or re-injury is present. Re-integrating children and youth into normal life and routines slowly, deliberately, and appropriately following a head injury involves two processes: return to learn and return to play.
Return to learn
Two fairly new recommendations apply to return to school and learning. First, medical clearance by a physician is no longer required to return to school, and second, children and youth should be encouraged to return to school as soon as possible, provided significant individualized supports are in place [7]. Several suitable ’return to learn’ templates with examples of supports are available for physicians, patients, and families. For an up-to-date summary on concussion return to learn and return to play please refer to Concussion Information on pedsconcussion.com.
Return to play
The early introduction of symptom-limited physical activity is appropriate. However, until a child or youth has returned to school successfully, they should not return to play with any risk of collision or falling [6]. Basic principles for returning to sport include: no return to play on the day a suspected injury occurs, return to play should follow a stepwise approach, and medical clearance is required before full-contact sport and game play can resume [7]. Full adherence to these guidelines is crucial to avoid aggravating symptoms and prevent secondary injuries before recovery is complete [26].
Prolonged symptoms
Individuals who experience prolonged symptoms require a multidisciplinary approach to care, with evaluation and management of any concurrent or contributing factors. Diagnostic testing and specific therapeutics are best managed by a physician or nurse practitioner with experience in treating prolonged concussion-related symptoms, as part of a multidisciplinary team if available. Specific evidence-based therapies directed by an HCP with expertise should be initiated and administered on an individualized basis and may include psychological treatments and cervical or vestibular rehabilitation, or both. Treatment should target specific symptoms, with focus on reducing stress, ensuring proper hydration, headache control, optimizing sleep, reducing screen-time, and maintaining an appropriate balance between rest and activity. The importance of healthy sleep habits cannot be overstated, with up to 85% of prolonged symptoms following head injury attributable in part to sleep dysfunction. Children and youth may also require psychosocial and emotional supports in the form of psychotherapy or cognitive-behavioral therapy (CBT) to treat injury-associated anxiety and depression [4][8]. Evidence is limited for the use of pharmacotherapy to treat concussion. Medications that target specific symptoms are sometimes used alongside careful return-to-play protocols [6][27]. Refer to the Living Guideline for a summary of treatment options [7].
Second impact syndrome (SIS)
SIS occurs when an individual experiences a second uncharacteristically severe head injury before recovering completely from concussion [28]. The pathophysiological processes involved in SIS are elusive and while the condition is rare, its consequences can be devastating, even leading to permanent disability or death. Risk for SIS underscores the importance of immediately removing any child or youth with suspected concussion from play, followed by a stepwise, supervised, gradual return to play or sport. Public health advocacy in the form of Rowan’s Law is one example of legislation that has increased concussion awareness, education, and safer return-to-play protocols.
Chronic traumatic encephalopathy (CTE) and retirement from sport
One highly controversial issue related to concussion is the long-term effects of repetitive head trauma. Concern is growing that recurrent concussions, or even sub-concussive blows, may cause a spectrum of complications known as CTE. CTE is a pathological diagnosis, and its clinical consequences are not yet fully known [6]. To date, epidemiological studies of children and youth who participate in contact and collision sports have not identified long-term neurological or psychiatric consequences. While the literature on neurobehavioural sequelae and long-term consequences from repeat injuries is inconsistent, the 5th International Consensus Statement on Concussion in Sport from 2016/17 stressed the risk for long-term effects from repeat injuries, including cognitive impairment and mental health problems. One retrospective cohort recently demonstrated a modest association between concussion experienced in childhood and subsequent risk for mental health issues, psychiatric hospitalizations, and self-harm [29]. There is still much to learn concerning the relationship between head injuries and development of CTE [6].
Having to retire from a sport they enjoy can have significant ramifications for child and youth mental and physical health, and data to guide when retirement is either necessary or appropriate are sparse. Taking a multidisciplinary, case-by-case approach that carefully weighs the risks and benefits of retirement alongside the individual athlete’s medical history, clinical status, and cognitive function, is recommended [8]. It remains unclear how many concussions are too many for the average child or youth, and the number of injuries is only one factor impacting long-term brain health and well-being [30][31]. Research addressing individualized risk-benefit models to guide informed decision-making about retirement or redirection from contact or collision sports is needed.
The role of bodychecking in head injury and concussion
Ice hockey is one of Canada’s most popular sports, with over 460,000 youth players registered in 2019/20. With lacrosse, hockey is considered a national sport, and the CPS acknowledges the historic, significant positive impacts of ice hockey for the mental, physical, and social health of Canadians. However, the relationship between bodychecking and injury in hockey has been studied for decades. The issue gained national prominence in 1989, after one powerful study found that bodychecking introduced at younger ages led to more aggressive play and higher penalty and injury rates [30]. Numerous studies have since confirmed a strong correlation between bodychecking and injury rates in children and youth [32]-[34]. A large dataset compiled over the 2005/16 period by the National High School Sports-Related Injury Surveillance Study found that 41.1% of hockey injuries were caused by bodychecking. Another study in 2011 followed 3000 boys aged between 4 and 18 years over a 5-year period and found that injury rates were 3 to 4 times higher in leagues that allowed bodychecking [30]. Injury rates in Canada have increased since and are expected to continue rising as players became larger, faster, and stronger [35].
Bodychecking is also a significant risk factor for concussion [36][37]. Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP) data from 2011/17 showed that ice hockey was the leading cause of all sports and recreationally related TBI across paediatric age groups, in both boys and girls, due in part to large participant numbers [3]. One meta-analysis of strategies to reduce concussion numbers estimated that eliminating bodychecking would decrease concussion rates in Canada by 20% to 90% in all age groups [38].
Subconcussive hits, meaning head injuries that do not produce a concussion but may have lasting effects on a developing brain, also warrant close attention. A 2014 study comparing male (bodychecking allowed) versus female (no bodychecking allowed) ice hockey players observed that males sustained a median 287 head impacts (interquartile range (IQR): 202-445) per season, while females received 170 (IQR: 119-230) [39].
Advanced video technology measuring “brain strain” provides further insight into the true impacts of bodychecking. Based on forces transmitted to the brain during bodychecking-related injuries, researchers are now advocating to remove bodychecking from the game altogether to reduce impact levels along the boards [40]. In 2021, one study recorded 172 games from six different age groups over a 2-year period and recreated the amount of head trauma in a laboratory setting. An increase in brain trauma when bodychecking was initiated was demonstrated [41].
Mounting evidence in both the United States (in 2012) and Canada (in 2013) led to a new policy that delayed the introduction of bodychecking until Bantam players reached 13 to 14 years of age (known now as U15). In 2014, the American Academy of Pediatrics (AAP) proposed restricting bodychecking to elite levels of boys’ hockey, starting no earlier than age 15 years [42]. Both the CPS and the AAP believe that delaying bodychecking is appropriate based not only on the significant variability in body maturation at this age but to decrease aggressive play [31][43].
The changes to bodychecking policy implemented by Hockey Canada and USA Hockey provided an opportunity to study the effects of reform on injury rates prospectively. Using National Electronic Injury Surveillance System (NEISS) data (for 2008/10 versus 2013/15), one study demonstrated that eliminating bodychecking in hockey had resulted in a 16.6% decrease in overall injury rates and a 38% decrease in bodychecking injuries in young players [44]. Another analysis of injury data in Canadian Pee Wee hockey players (under 13 years old) both before and after bodychecking rules changed, found a 50% relative reduction in injury rate and a 64% reduction in concussion rate [33].
More than 150 pre-eminent stakeholders in youth hockey met in 2017, with the aim of making hockey as safe as possible. After reviewing more than 40 scientific publications, they produced the official “Proceedings from the Ice Hockey Summit III: Action on Concussion”. Their goal was to “eliminate bodychecking in Bantam youth hockey games” [45].
Bodychecking in non-competitive play
Injury and concussion rates have been shown to be higher by three-fold among non-elite Pee Wee ice hockey players in leagues where bodychecking is permitted compared with leagues where bodychecking is prohibited [33]. One study compared injury rates between elite and non-elite Bantam players over a 2-year period (2014/16). The injury rate overall was 54% lower, and the severe injury rate was 61% lower, when bodychecking was disallowed for non-elite competitors. A 40% lower rate of concussion and a 45% lower rate of severe concussion were also observed, although these effects did not meet statistical significance. The study authors estimated that eliminating bodychecking for non-elite players could prevent 6386 injuries and 4340 severe injuries [32]. Another recent Canadian study found that disallowing bodychecking among non-elite 13- to 14-year-olds had reduced the rate of injuries by 4.32 per 1000 player-hours [46]. Health care costs were also examined, with an estimated 2.5 x reduction in health costs in leagues where bodychecking is disallowed among 11- to 12-year-olds [46]. This finding can be extrapolated to a cost-saving for Canada’s health care system of more than $1500 per 1000 player-hours [47].
Concussion prevention strategies
Despite the impacts of TBI and concussion specifically for individuals and society at large, public health strategies to decrease concussion risk remain elusive, in part because of the wide-ranging etiologies of, and mechanisms causing, head injuries [3].
Helmets
Systematic reviews of helmet use and concussion have been inconclusive. Helmets have been shown to decrease moderate to severe brain injuries, but their ability to decrease concussion risk has not been demonstrated [6][31]. Wearing head gear does not appear to reduce concussion risk in rugby and soccer, but helmets are strongly recommended for tackle football, ice hockey, lacrosse, downhill skiing, snowboarding, skateboarding, and bicycling to prevent moderate and severe brain injuries [31]. More research is needed to establish the efficacy of appropriate helmet wearing to prevent or mitigate concussive injuries.
Mouthguards
Evidence supporting the use of mouthguards to prevent concussions is mixed, but there has been a non-significant trend in support of protective effect when they are used in collision sports [30]. Mouthguards have been shown to decrease risk for dental and facial bone injuries and are recommended for high-risk activities. Research examining mouthguard use in contact sports is needed, but one meta-analysis suggested a 19% reduced risk of concussion when data from basketball, ice hockey, and rugby were combined [38].
Policy change
Policy change, rule enforcement, and education are the best evidence-based strategies to prevent head injuries [6][48]. Athletes, officials, administrators, parents, coaches, and HCPs all need to be aware and educated regarding risks for of SRC, its clinical features, assessment techniques, and the principles of safe return to play [6]. One meta-analysis analyzed concussion prevention strategies [49] including education, appropriate helmet use, and prohibiting bodychecking in hockey for younger players. Findings suggested that strengthening the neck muscles of young athletes may help prevent injury, but evidence was insufficient to support this as a strategy to decrease concussion risk [49].
Recommendations for health care providers
Health care professionals should:
- Be familiar with, and regularly update their knowledge of, current concussion management protocols. See ‘Recommended tools and resources’ below.
- Be aware of specific steps and timing for return-to-learn and return-to-play protocols.
- Be aware of and counsel families regarding risk factors for more severe injury and delayed recovery from concussion. Risk factors for a more severe injury include prolonged loss of consciousness, seizure activity, focal neurologic findings, and progressive or worsening symptoms Risk factors for prolonged recovery include multiple previous concussions, high symptom load at presentation, and applicable pre-existing or comorbid health issues (e.g., previous neurologic diagnosis, mental health issues, and social stressors). Expedite early referral for interdisciplinary care when any of these factors is present.
- Be aware of and counsel families regarding the clear associations between mental health and head injuries.
- Be aware of essential management steps when symptoms of concussion persist.
- Be aware that routine baseline neurocognitive testing and restrictive rest beyond the first 24 to 28 h are no longer required.
Recommendations for policy-makers
- Provincial/territorial governments should mandate schools (and those involved with school sports) and sports organizations to establish, update, and enforce policies and protocols to prevent, identify, and manage concussion.
- Canadian hockey organizations must implement policies and enforce rules to prevent bodychecking in all recreational leagues and play.
- Competitive hockey leagues must implement policies, training, and rules to prevent bodychecking before players are 15 years of age.
Recommended tools and resources
- Canadian Guideline on Concussion in Sport
- CATT Online – Concussion Awareness Training Tool
- Holland Bloorview Kids Rehabilitation Hospital - Concussion centre
- SCHOOLFirst: Enabling successful return-to-school following concussion
- Parachute – Concussion
- Parachute – Strategy for Return-to-School after a Concussion
- Parachute – After a Concussion: Return-to-Sport Strategy
- Parachute – Concussion Ed app
- PedsConcussion: Living Guideline for Pediatric Concussion Care
Acknowledgements
The authors wish to thank Pamela Fuselli and Stephanie Cowle for their review on behalf of Parachute Canada. This position statement has been reviewed by the Adolescent Health and Community Paediatrics Committees of the Canadian Paediatric Society.
CANADIAN PAEDIATRIC SOCIETY INJURY PREVENTION COMMITTEE
Members: Dominic Allain FRCPC MD, Émilie Beaulieu MD MPH, Suzanne Beno MD (Chair), Jeff Critch MD (Board Representative), Kristian Goulet MD, Daniel Rosenfield MD
Liaisons: André Champagne (Public Health Agency of Canada), Pamela Fuselli (Parachute - Leaders in Injury Prevention), April Kam MD (CPS Paediatric Emergency Medicine Section)
Principal authors: Kristian Goulet MD FRCPC, Suzanne Beno MD FRCPC
References
- McCrea M, Meier T, Huber D, et al. Role of advanced neuroimaging, fluid biomarkers and genetic testing in the assessment of sport-related concussion: A systematic review. Br J Sports Med 2017;51(12):919-29.
- Public Health Agency of Canada. Rausa VC, Shapiro J, Seal ML, et al. Neuroimaging in paediatric mild traumatic brain injury: A systematic review. Neurosci Biobehav Rev 2020;118:643-53.
- Release Notice – Injury in Review, 2020 edition: Spotlight on Traumatic Brain Injuries Across the Life Course. Health Promot Chronic Dis Prev Can 2020;40(9):294.
- Lumba-Brown A, Yeates KO, Sarmiento K, et al. Centers for Disease Control and Prevention guideline on the diagnosis and management of mild traumatic brain injury among children. JAMA Pediatr 2018;172(11):e182853.
- Purcell LK; Canadian Paediatric Society, Healthy Active Living and Sports Medicine Committee. Evaluation and management of children and adolescents with sports-related concussion. Paediatr Child Health 2012;17(1):31-34.
- McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport – The 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med 2017;51(11):838-47.
- Dawson J, Reed N, Bauman S, Seguin R, Zemek R. Diagnosing and managing paediatric concussion: Key recommendations for general paediatricians and family doctors. Paediatr Child Health 2021;26(7):402–07.
- Almeida AA, Lorincz MT, Hashikawa AN. Recent advances in pediatric concussion and mild traumatic brain injury. Pediatr Clin North Am 2018;65(6):1151-66.
- Zemek RL, Farion KJ, Sampson M, McGahern C. Prognosticators of persistent symptoms following pediatric concussion: A systematic review. JAMA Pediatr 2013;167(3):259-65.
- Davis GA, Purcell L, Schneider KJ, et al. The Child Sport Concussion Assessment Tool 5th Edition (Child SCAT5): Background and rationale. Br J Sports Med 2017;51(11):859-61.
- Schmidt J, Hayward KS, Brown KE, et al. Imaging in pediatric concussion: A systematic review. Pediatrics 2018;141(5):e20173406.
- Mannix R, Levy R, Zemek R, et al. Fluid biomarkers of pediatric mild traumatic brain injury: A systematic review. J Neurotrauma 2020;37(19):2029-44.
- Davis GA, Anderson V, Babl FE, et al. What is the difference in concussion management in children as compared with adults? A systematic review. Br J Sports Med 2017;51(12):949-57.
- Alsalaheen B, Stockdale K, Pechumer D, Broglio SP. Validity of the Immediate Post Concussion Assessment and Cognitive Testing (ImPACT). Sports Med 2016;46(10):1487-501.
- Barlow KM, Crawford S, Stevenson A, Sandhu SS, Belanger F, Dewey D. Epidemiology of postconcussion syndrome in pediatric mild traumatic brain injury. Pediatrics 2010;126(2):e374-81.
- Zemek R, Barrowman N, Freedman SB, et al. Pediatric Emergency Research Canada (PERC) Concussion Team. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA 2016;315(10):1014-25.
- Iverson GL, Gardner AJ, Terry DP, et al. Predictors of clinical recovery from concussion: A systematic review. Br J Sports Med 2017;51(12):941-48.
- Ponsford J, Nguyen S, Downing M, et al. Factors associated with persistent post-concussion symptoms following mild traumatic brain injury in adults. J Rehabil Med 2019;51(1):32-39.
- McNally KA, Bangert B, Dietrich A, et al. Injury versus noninjury factors as predictors of postconcussive symptoms following mild traumatic brain injury in children. Neuropsychology 201327(1):1-12.
- Belanger HG, Barwick FH, Kip KE, Kretzmer T, Vanderploeg RD. Postconcussive symptom complaints and potentially malleable positive predictors. Clin Neuropsychol 2013;27(3):343-55.
- Mittenberg W, DiGiulio DV, Perrin S, Bass AE. Symptoms following mild head injury: Expectation as aetiology. J Neurol Neurosurg Psychiatry 1992;55(3):200–04.
- Ferguson RJ, Mittenberg W, Barone DF, Schneider B. Postconcussion syndrome following sports-related head injury: Expectation as etiology. Neuropsychology 1999;13(4):582–89.
- Gunstad J, Suhr JA. ‘‘Expectation as etiology’’ versus ‘‘the good old days’’: Postconcussion syndrome symptom reporting in athletes, headache sufferers, and depressed individuals. J Int Neuropsychol Soc 2001;7(3):323–33.
- DeMatteo C, Bednar ED, Randall S, Falla K. Effectiveness of return to activity and return to school protocols for children postconcussion: A systematic review. BMJ Open Sport Exerc Med 2020;6(1): e000667.
- Ledoux AA, Barrowman N, Bijelić V, et al; PERC PedCARE Concussion team. Is early activity resumption after paediatric concussion safe and does it reduce symptom burden at 2 weeks post injury? The Pediatric Concussion Assessment of Rest and Exertion (PedCARE) multicentre randomised clinical trial. Br J Sports Med 2022;56(5):271-78.
- O’Neill JA, Cox MK, Clay OJ, et al. A review of the literature on pediatric concussions and return-to-learn (RTL): Implications for RTL policy, research, and practice. Rehabil Psychol 2017;62(3):300-23.
- Kuemmerle K, Meehan WP. Treatment of pediatric concussion. Semin Pediatr Neurol 2019;30:60-67.
- May T, Foris LA, Donnally CJ. Second impact syndrome. 2022 Jul 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
- Ledoux AA, Webster RJ, Clarke AE, et al. Risk of mental health problems in children and youths following concussion. JAMA Network Open 2022;5(3):e221235.
- Rivara FP, Tennyson R, Mills B, et al. Consensus statement on sports-related concussions in youth sports using a modified Delphi approach. JAMA Pediatr 2020;174(1):79-85.
- Régnier G, Boileau R, Marcotte G, et al. Effects of body-checking in Pee Wee (12 and 13 years old) division in the Province of Québec. In: Hoerner EF, ed. Safety in Ice Hockey. Philadelphia, PA: American Society for Testing and Materials; 1989.
- Emery C, Palacios-Derflingher L, Black AM, et al. Does disallowing body checking in non-elite 13- to 14-year-old ice hockey leagues reduce rates of injury and concussion? A cohort study in two Canadian provinces. Br J Sports Med 2020;54(7):414-20.
- Black AM, Hagel BE, Palacios-Derflingher L, Schneider KJ, Emery CA. The risk of injury associated with body checking among Pee Wee ice hockey players: An evaluation of Hockey Canada’s national body checking policy change. Br J Sports Med 2017;51(24):1767–72.
- Cusimano MD, Taback NA, McFaull SR, et al. Effect of bodychecking on rate of injuries among minor hockey players. Open Med 2011;5(1):e57-64.
- Darling SR, Schaubel DE, Baker JG, Leddy JJ, Bisson LJ, Willer B. Intentional versus unintentional contact as a mechanism of injury in youth ice hockey. Br J Sports Med 2011;45(6):492-97.
- Anderson GR, Melugin HP, Stuart MJ. Epidemiology of injuries in ice hockey. Sports Health 2019;11(6):514-19.
- Emery CA, Hagel B, Decloe M, Carly M. Risk factors for injury and severe injury in youth ice hockey: A systematic review of the literature. Inj Prev 2010;16(2):113-18.
- Emery CA, Black AM, Kolstad A, et al. What strategies can be used to effectively reduce the risk of concussion in sport? A systematic review. Br J Sports Med 2017;51(12):978-84.
- Wilcox BJ, Beckwith JG, Greenwald RM, et al. Head impact exposure in male and female collegiate ice hockey players. J Biomech 2014;47(1):109–14.
- Chen W, Post A, Karton C, Gilchrist MD, Robidoux M, Hoshizaki TB. A comparison of frequency and magnitude of head impacts between Pee Wee and Bantam youth ice hockey. Sports Biomech 2020:1-24. Online ahead of print.
- Karton C, Post A, Laflamme Y, et al. Exposure to brain trauma in six age divisions of minor ice hockey. J Biomech 2021;116:110203.
- Council on Sports Medicine and Fitness; Brooks A, Loud KJ, Brenner JS, et al. Reducing injury risk from body checking in boys' youth ice hockey. Pediatrics 2014;133(6):1151-57.
- McPherson MN, Montelpare W, Keightley M, et al. An analysis of head impact profiles and safe hockey behaviors in youth hockey players. J ASTM Int 2009;6(10):101908.
- Trofa DP, Park CN, Noticewala MS, Lynch TS, Ahmad CS, Popkin CA. The impact of body checking on youth ice hockey injuries. Orthop J Sports Med 2017;5(12):2325967117741647.
- Smith AM, Alford PA, Aubry M, et al. Proceedings from the Ice Hockey Summit III: Action on concussion. Clin J Sport Med 2021;31(3):e150–e160.
- Currie GR, Lee R, Palacios-Derflingher L, et al. Reality Check 2: The cost-effectiveness of policy disallowing body checking in non-elite 13- to 14-year-old ice hockey players. Int J Environ Res Public Health 2021;18(12):6322.
- Lacny S, Marshall DA, Currie G, et al. Reality check: The cost-effectiveness of removing body checking from youth ice hockey. Br J Sports Med 2014;48(17):1299-305.
- Cantu RC, Mueller FO. The prevention of catastrophic head and spine injuries in high school and college sports. Br J Sports Med 2009;43(13):981–86.
- Enniss TM, Basiouny K, Brewer B, et al. Primary prevention of contact sports-related concussions in amateur athletes: A systematic review from the Eastern Association for the Surgery of Trauma. Trauma Surg Acute Care Open 2018;3(1):e000153.
Disclaimer: The recommendations in this position statement do not indicate an exclusive course of treatment or procedure to be followed. Variations, taking into account individual circumstances, may be appropriate. Internet addresses are current at time of publication.

