Position statement
From ACEs to early relational health: Implications for clinical practice
Posted: Apr 3, 2023
Principal author(s)
Robin C. Williams MD; Canadian Paediatric Society,, Early Years Committee
Paediatr Child Health 2023 28(6):377–384. 
Abstract
Children grow and develop in an environment of relationships. Safe, stable, nurturing relationships help build resilience and buffer the negative impact of adverse experiences. Promoting relational health in clinical practice shifts the focus from adverse childhood experiences (ACEs) to positive childhood experiences (PCEs). This approach evaluates a family’s strengths and assets, and can be incorporated into both well-child and subspecialty care. While the optimal window for such interventions is in the prenatal period or as early as possible within the first 3 years of life, it is never too late to start. This statement describes how clinicians can bring a relational health approach to any medical encounter by understanding: what toxic stress is and how it can affect the developing brain, family relationships, and child development; how positive relationships, experiences, and behaviours can help buffer such effects and build resilience; observable signs of relational health and risk in parent-child interactions; the attributes of trustful, therapeutic relationships with families; and how to optimize these benefits through conversation and clinical practice.
Keywords: Adverse childhood experiences; Child development; Relational health; Resilience; Toxic stress
Introduction: From family deficits to relational strength
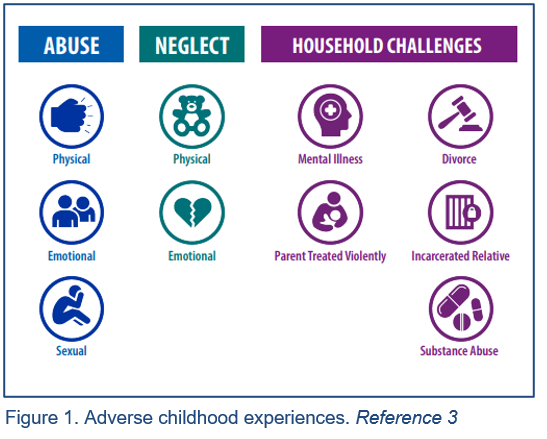
Since Felitti and Anda’s ground-breaking study on adverse childhood experiences (ACEs) nearly a quarter-century ago[1], paediatricians and other professionals caring for young children are increasingly aware of the negative, potentially lifelong effects that early life events can have on physical and mental health. As the literature connecting ACEs and health outcomes has grown, many clinicians working with adults have incorporated questions about childhood experiences into history-taking, adopting or adapting the original ACEs questionnaire to ask about the incidence of abuse, neglect, and household dysfunction in childhood[2][3] (see Figure 1). The cumulative ACEs “score” is then used as a proxy measure of risk and a tool to raise awareness that early experiences affect adult health and behaviour. Some paediatric clinics have also adopted this approach, asking not just about the experiences of patients but their parents (legal guardians, or other primary caregivers) as well, recognizing the impact that ACEs may have on parenting[4]-[6].
If ACEs help explain health or developmental challenges, early relational health provides a proactive pathway to mitigating them. A relatively new term for a not-so-new-concept, “early relational health” describes the emotional connections between children and trusted adults that promote health and development, lead to positive experiences, and can buffer the negative effects of trauma and adversity[7]-[10]. These safe, stable, and nurturing relationships (SSNRs) are foundational for building resilience, which is the ability to recover from stressors and negative experiences[8][9].
In addition to SSNRs, all children need to:
- Live, develop, play, and learn in safe, stable, protective, and equitable environments.
- Have opportunities for constructive social engagement to develop a sense of connectedness.
- Learn social and emotional competencies from caring adults[11].
These foundations of development depend on parenting skills, healthy routines, and community connections. Because parenting behaviours can be learned and modified, every visit is an opportunity to promote early relational health (ERH)[12]. ERH promotion involves strategies already used by paediatric health care providers such as directed history-taking, observing relationships[13], and active listening. It starts with evaluating a family’s strengths and assets, takes an antiracist and anti-oppressive perspective[14], and embraces these principles:
- The family—most broadly defined—is the child’s primary source of strength, support[15], and early learning[8].
- Paediatric health care providers are responsible for screening, assessing, and referring parents for physical, emotional, or social problems or health risk behaviours that may adversely affect children, or family life[15]-[18].
- Open, unbiased communication is key to a trusting therapeutic relationship[12] and involves: non-judgmental, empathetic listening and acceptance[8][19]; and eliciting parental observations, preferences, and input on what works best for their child[15][19][20].
- Clinicians should support parents’ involvement in children’s care management and decision-making[14] and in relational health care[8][9].
- Clinicians must continually mitigate their personal biases[13][21] by practicing cultural humility[14][20], honouring every family’s cultural identity and socio-economic background (Box 1), and considering them in health care planning and delivery. This type of care is collaborative and allows the family’s perspectives to become part of the health care plan[8][15][22].
Box 1. Cultural safety and cultural humility
Cultural safety is defined as what results when patients feel respected and safe in the health care system and in interactions with providers.
Cultural humility involves personal reflection to understand one’s own biases. It’s a lifelong process of learning to develop and maintain respectful processes and relationships based on mutual trust.
Reference 14
Ideally, relational health care process begins in the prenatal/perinatal period or during an early well-child visit, because the sooner a primary care provider can mitigate or prevent risk, the better the outcomes for children and families[9]. The optimal window for such interventions is early, within the first 3 years of life[23], but it is never too late to start[19][24].
This statement describes how clinicians can bring a relational health approach to all medical encounters by:
- Understanding what toxic stress is; how it can affect the developing brain, family relations, and child development; and how positive relationships, experiences, and behaviours can help buffer such effects[10].
- Watching for signs of relational health—and risk—in parent-child interactions.
- Appreciating the attributes of trustful, therapeutic relationships with families, and optimizing these benefits through conversation and practice.
- Identifying each family’s needs and referring them to community supports.
Biophysical effects of toxic stress and positive relationships
Life stressors are not always negative for children. With the help and support of caring adults, challenging experiences can help build resilience, teach coping strategies, strengthen family ties, and have positive impacts on family life. Brief periods of stress (such as the first day with a new caregiver or an immunization), when accompanied by the support of a caring and trusted adult, can positively affect children by building resilience[25].
But stress that is prolonged, persistent, and unbuffered by protective relationships with a caring adult can accentuate and reinforce toxic stress responses in children[26].
Unlike positive or tolerable stress (see Box 2), “toxic” stress activates “freeze, fight, or flight” responses for sustained periods, which can change the brain by altering networks in the amygdala, hippocampus, and prefrontal cortex. Over time, sustained exposure to toxic stress can lower the threshold for activating the stress response, causing it to respond more frequently than necessary or to remain stressed long after a threat has passed[27]. The brain becomes accustomed to scanning the environment for potential threats, releasing adrenalin and cortisol as it remains “on alert”.
Box 2. Types of stress
Positive stress is brief, and can result from common or unfamiliar experiences such as starting child care or getting a vaccine. The body may respond with a brief increase in heart rate, and mild to moderate increases in stress hormones like adrenaline and cortisol.
Tolerable stress can last longer and result from more serious life events, such as injury, death or divorce, or natural disaster. Supportive, caring adults can maintain a safe environment and help children cope by ensuring that their physical and emotional responses to more serious events remain tolerable.
Toxic stress typically arises from situations such as abuse or neglect, where children do not receive support from caring adults.Toxic stress may be frequent or chronic and—in the absence of relationships that buffer the impact—can affect brain development.
Reference 27
Chronic activation of the stress-response system can affect both the brain and the body, including the endocrine, immune, and nervous systems[4][28][29]. Areas of the brain related to executive function—memory, learning, decision-making, and stress response—can also become impaired[4].
However, brain imaging has also shown the development of a highly protective “biobehavioural synchrony” between infants and parents, where close, social contact results in a dynamic exchange of hormonal, physiological and behavioural cues that support children’s physical and social growth[30]. Positive reciprocal experiences—exchanges of gaze, touch, vocalizations, and affect between parent and infant—predict a child’s ability to self-regulate, manage stress, and feel empathy[30], and support other key aspects of development including secure attachment, autonomy, perspective-taking, and problem- solving.
How childhood experiences affect parenting
A parent’s capacity for nurturing behaviours depends in part on nervous system and hypothalamic-pituitary-adrenal (HPA) axis function, and living with the sequelae of multiple ACEs can negatively affect both[4]. Chronic toxic stress can overload an individual’s stress response system[28], causing them to be more likely to misperceive threats and react angrily to, or withdraw emotionally from, challenging child behaviours or stressful family situations[28][29].
Multiple studies have associated significant adversity experienced in childhood with suboptimal parenting skills in later life[12][31]:
- Adults who have experienced 4 or more ACEs are at increased risk for mental health problems and parenting difficulties[18][32][33], including a four-fold greater risk for depression[4][34].
- Mothers living with multiple ACEs or depression (which is in turn associated with ACE history[35]-[37]) may be less attuned and responsive to the needs of their infants, and less available psychologically or emotionally to young children[32][35][38]-[41].
- Maternal ACE exposure can lead to attachment insecurity, with negative effects on social-emotional function in infants and young children[17]. (While most of the evidence in this area involves mothers, the effects of ACE exposure may be similar for all primary caregivers, including fathers.)
Parents who experienced ACEs may not be aware of how their history affects current family life and relationships[5], but making this connection can break cycles of negativity. A parent who experienced trauma in childhood may be less able to practice adequate self-care, recognize when they need help and ask for it, provide developmentally appropriate discipline, model appropriate conflict resolution at home, or even play with their child[6]. Parents who have difficulty modulating their own stress responses may have trouble helping children adapt to life’s stressors[25][32]. Finally, adults who experienced harsh parenting (eg., shouting, physical punishment) as children are more likely to engage in harsh parenting themselves[6][42].
Evidence is growing that family-based interventions to promote parental sensitivity can help mitigate or interrupt the intergenerational effects of ACEs and extend a parent’s own early life resilience to their children[17][31]. HPA axis function and stress hormone regulation in children have been shown to respond positively to early interventions, and even to normalize when parenting practices have changed[12]. Positive childhood experiences have been shown to help mitigate the effect of ACEs[10].
Effects on child development
Even before children are born, a persistently hyperactive maternal stress response during pregnancy may increase fetal developmental risk via epigenetic and neurobiological mechanisms[17][32][43]. For example, infants whose mothers experience chronic stress from racial discrimination may be at risk for poor outcomes such as low birth weight, or infants born preterm or small for gestational age[44][45].
In early childhood, parental ACEs can negatively affect development in areas such as problem-solving, communication, and personal-social and motor skills[17][29]. The number of parental ACEs has been directly correlated to a child’s developmental screen results at age 2 years[29].
Developmental risk in children is associated particularly strongly with maternal ACEs, and can be compounded further by maternal depression[36][37]. Two Canadian studies directly associated maternal ACEs with delayed achievement of children’s milestones at 12 months and increased risk for parent-child relationship difficulties in infancy[32][46]. Researchers have also found a dose-response relationship between the number of maternal ACEs and risk for developmental delay in communication and gross and fine motor skills at 24 months of age, particularly if family protective factors were low[17]. More maternal ACEs, which can undermine mental health, have also been associated with infant emotional dysfunction at 6 and 18 months of age[17], and risk of missing well-child visits in the first 2 years, with consequent delays in developmental screening, guidance, and referral for services[47].
There is increasing evidence that family resilience and connection, and positive relational experiences, build resilience throughout childhood, even in the face of adversity[9][10]. Resilience includes individual capacity, nurturing relationships, access to resources, systems, and personal skills that allow children and families to respond to adversity in healthy, adaptive ways[9][10]. Personal social skills such as emotional regulation and executive function (e.g., impulse inhibition, working memory, cognitive flexibility, planning, and problem-solving) can be modeled, taught, learned, practiced, reinforced, and celebrated in children and parents[9].
Assessing relational health in clinical practice
Multiple studies have demonstrated the benefits of pre-emptive parental assessment and guidance. For example, inquiry and counselling during pregnancy and the perinatal period around effective parenting skills[4][48][49], especially when reinforced by evidence-based home visiting services (e.g. by public health nurses)[19][24], has been shown to decrease parental stress, enhance maternal mental health, and help break intergenerational transmission of risk for ACEs[48]-[51].
Box 3. Discuss, model, praise
Developers of the Keystones of Development curriculum recommend a three-step approach to promoting early relational health in clinical practice:
- Discuss the specific parenting behaviours that support the concept (e.g., noticing and responding to baby’s cues helps promote secure attachment).
- Model the behaviours during the visit (e.g., through warm, back-and-forth interactions).
- Praise what you observe (e.g., the baby calms down when the parent holds them).
Adapted from reference 54
Relational health assessment should always begin with reflective self-assessment by primary care providers. Recognizing the personal biases that they may bring to practice is an essential first step[19][20][52], and is discussed in more detail below. Next, the relational assessment checks that children have at least one caring, supportive, and emotionally available adult in their life[11][19][20], and builds from there. In a clinical setting, a secure parent-child attachment may be implied through mutual parent-child attraction, vocal communication, facial expressions, and sensitivity/reciprocity of response[13][53], remembering that positive affect and interactions—especially non-verbal behaviours—can look somewhat different across cultures or when a child has a developmental disorder that affects communication[22]. Secure attachment will be most evident when a child is hurt, sick, or afraid, turns to their adult, and the adult responds with warmth and comfort.
Relational assessment involves observing and talking about positive aspects of a parent’s past and family history and can be inherently therapeutic[33]. See (Box 3) for an example of this approach[54]. Being attentive over time to the family’s capacity to provide safe, stable, nurturing relationships and environments can reinforce their strengths, promote relational health, and help mitigate or prevent stress[8]. These conversations also help clinicians build supportive, trustful practitioner-parent relationships, improve the quality of health care interactions overall, enhance understanding of any underlying causes of physical and mental health problems, and ensure more effective treatment planning[4][5][12][17][33][55]. Understanding to what degree families are part of communities, and what support they receive, could be another opportunity for connection.
Relational, trauma-informed care underscores the importance of actively listening to parents without bias. With input from parents, clinicians should assess for:
- Safe, stable, and nurturing relationships (e.g., warm parent-child interactions every day)[23][48][56].
- Positive relationships with second caregivers, extended family, or other caring adults[48], which can buffer against the intergenerational transmission of maltreatment[43].
- Family-specific strengths, such as closeness, support, loyalty, protection, and love[48].
- Community engagement (e.g., library programs, child care centres, recreational facilities, schools, culturally specific programs)[23]. Local public health departments often have links to community resources.
Each clinical encounter is an opportunity to promote parenting behaviours that will help children develop secure attachment, autonomy, self-regulation, perspective-taking, and problem-solving—all of which are strongly predictive of later well-being[54].
Building relational health through guidance, treatment, and practice culture
While it is increasingly recognized that ACEs may affect not only the individuals who live them, but subsequent generations[4][16][25][32][38][55], evidence also suggests the parent-child relationship is a leading and modifiable mechanism for transmitting both risk[4] and resilience[10][19]. ACEs, patient- and family-centred, and relational models all recommend taking a two-generation approach to care[9][31][38], with the experiences of children as a constant, central focus[4][8].
Reassuring messages to counsel and reinforce with parents and caregivers include the following:
- Caring parents can buffer stress and build resilience in children, even in difficult circumstances or when they have experienced ACEs themselves[10][12][57][58].
- Challenging behaviours in both parents and children may be survival or adaptive coping strategies against early stressors[19].
- Although healthy family routines may differ culturally, they typically build resilience by making children feel safe and providing parents with perspective and a sense of autonomy. They have also been shown to mitigate toxic stress and neuroendocrine activation in young children (measured by salivary cortisol levels)[12].
- Shared reading nurtures relational health in myriad ways[59].
- Healthy sleep routines—which may look different across cultures—appear to protect children’s social-emotional and behavioural development even when maternal mental health is problematic[56].
- Parent-child relationships are built on connective moments: not only of spontaneous delight, but the intentional sharing of comfort and meaning in times of disruption and repair[53].
- Feeling frustrated is a normal part of parenting, but knowledge and coping strategies such as physical exercise, mindfulness, deep breathing, psychotherapy, cognitive behavioural therapy (CBT) techniques, community connections, and healthy family routines can help[4][12][13][60]-[62].
- Parental self-care is important[12]. Sleep routines, self-settling strategies, and stress management techniques[56] are opportunities to pause, relax, and refresh, and are skills to model for children[63].
Relational health care also depends on flexible office practices that involve parents and ensure they have opportunities to talk about difficulties with health care providers and staff[4][12][19][20][29]. Trauma-informed approaches should be learned, practiced, and modelled for families by all staff. For example:
- Recognize, acknowledge, and validate specific family struggles—even when they are difficult to modify or influence, such as racism, systemic oppression, and poverty[8][52].
- Respect parents as experts in their lived experience, and invite them to guide discussion, establish boundaries, and choose next steps for care management or treatment planning[4][20][22][55].
- Promote protective family factors (e.g., SSNRs, healthy routines, culture, community) [13][15][19][20][24][29][62] as empowering, supportive, and predictive of resilience. Consider siblings, extended family, peers, teachers, neighbours, elders, and other community leaders[18][20][48].
- Ensure that health care information is clear, complete, objective, inclusive, and unbiased, as well as useful and affirming[15]. Involve a professional translator or cultural navigator when needed.
- Health information and updates should be shared in a family’s chosen language, with compassion, in culturally safe and respectful ways, and at a level compatible with parental health literacy[15].
The relational health model proposes working across sectors and teams, integrating mental health and behavioural counselling into clinic settings, and making space for cultural practices whenever possible[19][20]. To treat suspected attachment disorders or attachment insecurity, anxiety, oppositional defiant disorder, or post-traumatic stress disorder in young children, consider referral for: attachment and biobehavioural catch-up (ABC), parent-child interaction therapy (PCIT), child-parent psychotherapy (CPP), or attachment-focused parent psychoeducation groups like Circle of Security[9].
Maintaining updated listings for community-based services and parenting programs to facilitate referrals[4][12] is essential. Public health and municipal services can be useful places to start.
Community-based agencies that serve children, such as schools, libraries, and early intervention programs[62] can help families build connections with others of similar cultural or linguistic background, find peer-to-peer support, and access targeted services such as home visiting programs[15][19][24]. To encourage parental well-being, counsel on options such as local parenting groups, mindfulness or exercise classes, psychotherapy, or engagement with friends and family[62]. Holistic, team-based care approaches with links to community could allow more time and space for health promotion[53], or the delivery of services and programs that have been co-developed by the families and communities they serve[8][20].
Recommendations
For clinical practice
Over time, paediatricians and other primary care providers can assess and build on family strengths to help prevent and mitigate risk from adverse childhood experiences (ACEs). They should support and promote key drivers of early relational health and development for all children, in all families, in all settings. These drivers include:
- Safe, stable, nurturing relationships (SSNRs) with parents, alternate caregivers, siblings, and extended family. SSNRs are signaled by a secure attachment or serve-and-return interactions.
- Parental health and well-being.
- Breastfeeding, positive parenting, early literacy, quality child care and education, and developmentally appropriate play.
- Connection with community resources, including pre- and post-natal home visiting programs, early child development programs, libraries, cultural networks, and play groups.
Health care professionals should use each clinical encounter to discuss, model, and praise specific parenting behaviours that promote early relational health and contribute to the development of secure attachment, autonomy, self-regulation, perspective-taking, and problem-solving.
After considering their own biases, primary care providers should assess relational health by observing parent-child interactions, listening closely to parents, and asking about:
- Parental, family, and community history;
- Their experience of parenting;
- Healthy relationships between parenting partners;
- Child behaviours and how they respond;
- Positive, protective family routines and parenting practices; and
- Any stressors at home (e.g., financial, food insecurity, housing, violence).
When the family raises relationship concerns, consider the following interventions:
- Counselling on healthy parenting strategies.
- Connecting parents with culturally safe community services, pre- and post-natal home visiting programs, peer-to-peer support groups, and parenting programs. Contact local public health for information on community resources.
- Screening and appropriate referrals for postpartum mood disorders, intimate partner violence, mental health risk, or substance misuse.
For health care settings
Physicians and staff should be trained to deliver family-centred, antiracist, anti-oppressive, and trauma-informed care at every interaction by:
- Integrating mental health counselling (including community partners such as psychologists and social workers) with clinic settings whenever possible,
- Acknowledging and addressing personal biases and barriers to health care facing the families they serve,
- Being compassionately available and easily accessible, and
- Being culturally sensitive, responsive, and inclusive.
For medical education
Medical school and residency curriculums as well as continuing education programs should provide enhanced training in early child development, specifically:
- The importance of early relational health for child development and parenting behaviours.
- Family environments and parenting behaviours that foster early relational health and strengthen resilience by promoting secure attachment, autonomy, self-regulation, perspective-taking, and problem-solving.
- Adverse childhood experiences (ACEs) and toxic stress effects on physical health and mental well-being, in childhood and longer term.
- Evidence-based strategies to mitigate or prevent the risks associated with ACEs.
One example of an evaluated program to teach the relational approach to both learners and physicians in practice is the Keystones of Development (https://parenting.mountsinai.org/providers/).
For health policy
Provincial and territorial governments can support early relational health promotion by:
- Encouraging the development of and providing funding for local programs and services that support parents and prioritize relational health.
- Adjusting payment structures to support extra in-clinic time for targeted conversations with families.
Acknowledgements
This statement was reviewed by the following Canadian Paediatric Society groups: Social Paediatrics and Community Paediatrics Section executives; Community Paediatrics Committee; First Nations, Inuit and Métis Health Committee; and Mental Health and Developmental Disabilities Committee. Thanks to Dr. Richa Agnihotri, Dr. Sara Citron, Dr. Benjamin Klein, and the Niagara Region Family Health team for their careful review, and to Jennie Strickland for statement drafting.
CANADIAN PAEDIATRIC SOCIETY EARLY YEARS TASK FORCE (2022-23)
Members: Sanjeev Bhatla MD (College of Family Physicians of Canada); Jean Clinton MD; Andrea Feller MD; Emmett Francoeur MD; Kassia Johnson MD; Katherine Matheson MD (Canadian Academy of Child and Adolescent Psychiatry); Annie Murphy Savoie MD; Alyson Shaw MD; Robin C. Williams MD (Chair)
Principal author: Robin C. Williams, MD
References
- Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. Am J Prev Med 1998;14(4):2450-58. doi: 10.1016/S0140-6736(12)60072-5.
- Schulman M, Maul A, Center for Health Care Strategies. Screening for Adverse Childhood Experiences and Trauma. February 2019: https://www.chcs.org/media/TA-Tool-Screening-for-ACEs-and-Trauma_020619.pdf (Accessed February 22, 2023).
- Centers for Disease Control and Prevention. Adverse Childhood Experiences Prevention Strategy. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 2021 (Accessed February 22, 2023).
- Gupta RC, Randell KA, Down MD. Addressing parental adverse childhood experiences in the pediatric setting. Adv Pediatr 2021;68:71-88. doi: 10.1016/j.yapd.2021.05.003.
- Gillespie RJ. Pediatric Cases: Examples of Screening in Action. In: Applying the Science of Toxic Stress to Support Children's Health. April 14, 2021: https://www.acesaware.org/wp-content/uploads/2021/04/April-14-Supporting-Childrens-Health-Slide-Deck.pdf (Accessed February 22, 2023).
- Gillespie RJ. Assessing parental ACEs in Primary Care Pediatrics: What We’ve Learned, and How Practice has Changed. Academy on Violence and Abuse (AVA) pre-conference, San Diego, CA. January 2020. Slidedeck: https://www.avahealth.org/file_download/943a67ff-6788-48df-a02c-9b709669710c (Accessed February 22, 2023).
- Burstein D, Yang C, Johnson K, Linkenbach J, Sege R. Transforming practice with HOPE (Healthy Outcomes from Positive Experiences). Matern Child Health J 2021;25(7):1019-24. doi: 10.1007/s10995-021-03173-9.
- Willis DW, Pardis N, Johnson K. The Paradigm Shift to Early Relational Health: A Network Movement. May 31, 2022: https://www.zerotothree.org/resources/4420-the-paradigm-shift-to-early-relational-health-a-network-movement (Accessed February 22, 2023).
- Garner A, Yogman M, AAP Committee on Psychosocial Aspects of Child and Family Health, Section on Developmental and Behavioral Pediatrics, Council on Early Childhood. Preventing childhood toxic stress: Partnering with families and communities to promote relational health. Pediatrics 2021;148(2):e2021052582. doi: 10.1542/peds.2021-052582.
- Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. positive childhood experiences and adult mental and relational health in a statewide sample: associations across adverse childhood experiences levels. JAMA Pediatr 2019;173(11):e193007. doi:10.1001/jamapediatrics.2019.3007.
- Sege RD, Browne CH. Responding to ACEs with HOPE: Health outcomes from positive experiences. Acad Pediatr 2017;17(7S):S79-S85. doi: 10.1016/j.acap.2017.03.007.
- Traub F, Boyton-Jarrett R. Modifiable resilience factors to childhood adversity for clinical pediatric practice. Pediatrics 2017;139(5):e20162569. doi: 10.1542/peds.2016-2569.
- Forkey H. Putting your trauma lens on. Pediatr Ann 2019;48(7):e269-73.
- First Nations Health Authority (B.C.). Cultural Safety and Humility: https://www.fnha.ca/wellness/wellness-and-the-first-nations-health-authority/cultural-safety-and-humility (Accessed February 22, 2023).
- American Academy of Pediatrics; Committee on Hospital Care and Institute for Patient- and Family-centered Care. Policy statement: Patient- and family-centered care and the pediatrician’s role. Pediatrics 2012;129(2):394-404. doi: 10.1542/peds.2011-3084.
- Ford K, Hughes K, Hardcastle K, et al. The evidence base for routine enquiry into ACEs: A scoping review. Child Abuse and Negl 2019;91:131-46. doi: 10.1016/j.chiabu.2019.03.007.
- Folger AT, Eismann EA, Stephenson NB, et al. Parental adverse childhood experiences and offspring development at 2 years of age. Pediatrics 2018;14(4):e20172826. doi: 10.1542/peds.2017-2826.
- Murphy A, Steele M, Dube SR, et al. Adverse childhood experiences (ACEs) questionnaire and adult attachment interview (AAI): Implications for parent child relationships. Child Abuse Negl 2014;38(2):224-33. doi: 10.1016/j.chiabu.2013.09.004.
- Forkey H, Szilagyi M, Kelly ET, Duffee J; AAP Council on Foster Care, Adoption, and Kinship Care, Council on Community Pediatrics, Council on Child Abuse and Neglect, Committee on Psychosocial Aspects of Child and Family Health. Trauma-informed care. Pediatrics 2021;148(2):e2021052580. doi: 10.1542/peds.2021-052580.
- Duffee J, Szilagyi M, Forkey H, Kelly ET; AAP Council on Community Pediatrics, Council on Foster Care, Adoption, and Kinship Care, Council on Child Abuse and Neglect, Committee on Psychosocial Aspects of Child and Family Health. Trauma-informed care in child health systems. Pediatrics 2021;148(2):e2021052579. doi: 10.1542/peds.2021-052579.
- Ward MGK, Baird B; Canadian Paediatric Society, Child and Youth Maltreatment Section. Medical neglect: Working with children, youth, and families. Paediatr Child Health 2022;27(6):372-76:https://cps.ca/en/documents/position/medical-neglect
- Charlot-Silley D, Condon MC, Rahman T. At the feet of storytellers: Implications for practicing early relational health conversations. Infant Ment Health J 2022;43(3):378-89. doi: 10.1002/imhj.21981.
- McDonald S, Kehler H, Bayrampour H, Fraser-Lee N, Tough S. Risk and protective factors in early child development: Results from the All Our Babies (AOB) pregnancy cohort. Res Dev Disabil 2016;58:20-30. doi: 10.1016/j.ridd.2016.08.010.
- Hambrick EP, Bawner TW, Perry BD, Brandt K, Hofmeister C, Collins JO. Beyond the ACE score: Examining relationships between timing of developmental adversity, relational health and developmental outcomes in children. Arch Psychiatr Nurs 2019;33(3):238-47. doi: 10.1016/j.apnu.2018.11.001.
- Szilagyi M, Kerker BD, Storfer-Isser A, et al. Factors associated with whether pediatricians inquire about parents’ ACEs. Acad Pediatr 2016;16(7):668-75. doi: 10.1016/j.acap.2016.04.013.
- Harvard University. Center on the Developing Child. Key Concepts. Toxic Stress: https://developingchild.harvard.edu/science/key-concepts/toxic-stress/ (Accessed February 22, 2023).
- National Scientific Council on the Developing Child (2005/2014). Excessive Stress Disrupts the Architecture of the Developing Brain: Working Paper No. 3. Updated edition, January 2014: https://developingchild.harvard.edu/resources/wp3/ (Accessed February 22, 2023).
- Thakur N. Stress and ACEs: Risk Factors for Poor Health. In: ACEs Aware. Applying the Science of Toxic Stress to Support Children’s Health. April 14, 2021: https://www.acesaware.org/wp-content/uploads/2021/04/April-14-Supporting-Childrens-Health-Slide-Deck.pdf (Accessed February 22, 2023).
- Bernard-Pearl D, Gillespie RJ, Marie-Mitchell A; PACES Connection Staff. Integrating ACE Science in Pediatrics: Early Adopters. Webinar, October 17, 2019: https://www.pacesconnection.com/blog/how-do-these-pediatricians-do-aces-screening-early-adopters-tell-all (Accessed February 22, 2023).
- Feldman R. The adaptive human parental brain: Implications for children’s social development. Trends Neurosci 2015;38(6):387–99. doi: 10.1016/j.tins.2015.04.004.
- Bifulco A, Moran PM, Ball C, et al. Childhood adversity, parental vulnerability and disorder: Examining inter-generational transmission of risk. J Child Psychol Psychiatry 2002;43(8):1075-86. doi: 10.1111/1469-7610.00234.
- Madigan S, Wade M, Plamondon A, Maguire JL, Jenkins JM. Maternal adverse childhood experience and infant health: Biomedical and psychosociall risks as intermediary mechanisms. J Pediatr 2017;187:282-89.e. doi: 10.1016/j.jpeds.2017.04.052.
- Goldstein E, Athale N, Sciolla AF, Catz SL. Patient preferences for discussing childhood trauma in primary care. Perm J 2017;21:16-55. doi: 10.7812/TPP/16-055.
- Marie-Mitchell A, Studer KR, O’Connor TG. How knowledge of adverse childhood experiences can help pediatricians prevent mental health problems. Fam Syst and Health 2016;34(2):128-35. doi: 10.1037/fsh0000179.
- Steven K. Exploring parent perception of adverse childhood experiences screening in pediatric primary care: A clinical inquiry project. Fayetteville, AR: The Eleanor Mann School of Nursing Student Works, 2021: https://scholarworks.uark.edu/cgi/viewcontent.cgi?article=1013&context=nursstudent (Accessed February 22, 2023).
- Sun J, Patel F, Rose-Jacobs R, Frank DA, Black MM, Chilton M. Mothers’ adverse childhood experiences and their young children’s development. Am J Prev Med 2017;53(6):882-91. doi: 10.1016/j.amepre.2017.07.015.
- Kingston D, Tough S. Prenatal and postnatal maternal mental health and school-age child development: A systematic review. Matern Child Health J 2014;18(7):1728-41. doi: 10.1007/s10995-013-1418-3.
- Lê-Scherban F, Wang X, Boyle-Steed KH, Pachter LM. Intergenerational associations of parent adverse childhood experiences and child health outcomes. Pediatrics 2018;14(6):e20174274. doi: 10.1542/peds.2017-4274.
- Lang AJ, Gartstein MA, Rodgers CS, Lebeck MM. The impact of maternal childhood abuse on parenting and infant temperament. J Child Adolesc Psychiatr Nurs 2010;23(2):100-10. doi: 10.1111/j.1744-6171.2010.00229.x.
- Kim P. How stress can influence brain adaptations to motherhood. Front Neuroendocrinol 2021;60:100875. doi: 10.1016/j.yfrne.2020.100875.
- Madigan S, Wade M, Plamondon A, Jenkins J. Maternal abuse history, postpartum depression, and parenting: Links with preschoolers’ internalizing problems. Infant Ment Health J 2015;36(2):146-55. doi: 10.1002/imhj.21496.
- Dowd MD. The relevance of parental adverse childhood experiences in pediatric practice. Pediatr Ann 2019;48(12):e463-65. doi: 10.3928/19382359-20191118-03.
- Plant DT, Pawlby S, Pariante CM, Jones FW. When one childhood meets another—maternal childhood trauma and offspring child psychopathology: A systematic review. Clin Child Psychol Psychiatry 2018;23(3):483-500. doi: 10.1177/1359104517742186.
- Larrabee Sonderlund A, Schoenthaler A, Thilsing T. The association between maternal experiences of interpersonal discrimination and adverse birth outcomes: A systematic review of the evidence. Int J Environ Res Public Health 2021;18(4):1465. doi: 10.3390/ijerph18041465.
- Alhusen JL, Bower KM, Epstein E, Sharps P. Racial discrimination and adverse birth outcomes: An integrative review. J Midwifery Womens Health 2016;61(6):707-20. doi: 10.1111/jmwh.12490.
- Racine N, Plamondon A, Madigan S, McDonald S, Tough S. Maternal adverse childhood experiences and infant development. Pediatrics 2018;141(4):e20172495. doi: 10.1542/peds.2017-2495.
- Eismann EA, Folger AT, Stephenson NB, et al. Parental adverse childhood experiences and pediatric healthcare use by 2 years of age. J Pediatr 2019;211:146-51. doi: 10.1016/j.jpeds.2019.04.025.
- Narayan AJ, Rivera LM, Bernstein RE, Harris WW, Lieberman AF. Positive childhood experiences predict less psychophatholy and stress in pregnant women with childhood adversity: A pilot study of the benevolent childhood experiences (BCEs) scale. Child Abuse Negl 2018;78:19-30. doi: 10.1016/j.chiabu.2017.09.022.
- Schickedanz A, Halfon N, Sastry N, Chung PJ. Parents’ adverse childhood experiences and their children’s behavioural health problems. Pediatrics 2018;142(2):e20180023. doi: 10.1542/peds.2018-0023.
- McDonnell CG, Valentino K. Intergenerational effects of childhood trauma: Evaluating pathways among maternal ACEs, perinatal depressive symptoms, and infant outcomes. Child Maltreat 2016;21(4):317-26. doi: 10.1177/1077559516659556.
- Seng JS, Sperlich M, Rowe H, et al. The survivor mom’s companion: Open pilot of a posttraumatic stress specific psychoeducation program for pregnant survivors of childhood maltreatment and sexual trauma. Int J Childbirth 2011;1(2):11-21. doi: 10.1891/2156-5287.1.2.111
- Gerlach AJ, Browne AJ, Suto MJ. Relational approaches to fostering health equity for Indigenous children through early childhood intervention. Health Sociol Rev 2018;27(1):104-19. doi: 10.1080/14461242.2016.1231582.
- Willis DW. Early Relational Health (ERH): An Introduction. June 12, 2019. Webinar: Center for the Study of Social Policy: https://cssp.org/wp-content/uploads/2019/06/Early-Relational-Health-Webinar-6.12.19.pdf (Accessed February 22, 2023).
- Hammond BS. Promoting early relational health and child development in Canadian resident education and clinical practice moments. February 9, 2023. Webinar: Canadian Paediatric Society: https://cps.ca/en/strategic-priorities/early-child-development (Accessed February 13, 2023).
- Gillespie RJ, Folger AT. Feasibility of assessing parental ACEs in pediatric primary care: Implications for practice-based implementation. J Child Adol Trauma 2017;10:249-56. doi: 10.1007/s40653-017-0138-z.
- McDonald SW, Kehler HL, Tough SC. Protective factors for child development at age 2 in the presence of poor maternal mental health: Results from the All Our Babies (AOB) pregnancy cohort. BMJ Open 2016;6(11):e012096. doi: 10.1136/bmjopen-2016-012096.
- Burke Harris N. The Deepest Well: Healing the Long-term Effects of Childhood Adversity. New York, NY: Houghton Mifflin Harcourt, 2018.
- Morris AS, Robinson LR, Hays-Grudo J, Claussen AH, Hartwig SA, Treat AE. Targeting parenting in early childhood: A public health approach to improve outcomes for children living in poverty. Child Dev 2017;88(2):388–97. doi: 10.1111/cdev.12743.
- Shaw A; Canadian Paediatric Society, Early Years Task Force. Read, Speak, Sing: Promoting early literacy in the health care setting. January 2021:https://cps.ca/en/documents/position/read-speak-sing-promoting-literacy
- Hudziak JJ. ACEs and pregnancy: Time to support all expectant mothers. Pediatrics 2018;14(4):e20180232. doi: 10.1542/peds.2018-0232.
- Davis DW, Myers J, Logsdon MC. Bauer NS. The relationship among caregiver depressive symptoms, parenting behaviour, and family-centered care. J Pediatr Health Care 2016;16(7):668-75. doi: 10.1016/j.pedhc.2015.06.004.
- Bair-Merritt MH, Zuckerman B. Exploring parents’ adversities in pediatric primary care. JAMA Pediatr 2016;170(4):313-14. doi: 10.1001/jamapediatrics.2015.4459.
- Center for the Study of Social Policy. Building Resilience in Troubled Times: A Guide for Parents: https://cssp.org/building-resilience-in-troubled-times-a-guide-for-parents/ (Accessed February 22, 2023).
Disclaimer: The recommendations in this position statement do not indicate an exclusive course of treatment or procedure to be followed. Variations, taking into account individual circumstances, may be appropriate. Internet addresses are current at time of publication.

