Position statement
Managing type 1 diabetes in school: Recommendations for policy and practice
Posted: Feb 6, 2015
Principal author(s)
Sarah E Lawrence MD, Elizabeth A Cummings MD, Danièle Pacaud MD, Andrew Lynk MD, Daniel L Metzger MD
Paediatr Child Health 2015;20(1):35-39.
Abstract
Diabetes requiring insulin is increasingly common and likely to impact students in most, if not all, schools. Diabetes and its complications have major personal, social and economic impact, and improved diabetes control reduces the risk of both short- and long-term complications. Evidence shows that more intensive management of diabetes – through frequent blood glucose monitoring, insulin administration with injections and/or insulin pumps, and careful attention to diet and exercise – leads to better control. Since children spend 30 to 35 hours per week at school, effectively managing their diabetes while there is integral to their short- and long-term health. The Canadian Paediatric Society and the Canadian Pediatric Endocrine Group recommend that minimum standards for supervision and care be established across Canada to support children and youth with type 1 diabetes in schools. These recommendations are derived from evidence-based clinical practice guidelines, with input from diabetes care providers from across Canada, and are consistent with the Canadian Diabetes Association’s Guidelines for the Care of Students Living with Diabetes at School.
Key Words: Education; Policy; Type 1 diabetes
The Canadian Paediatric Society and the Canadian Pediatric Endocrine Group are concerned about how type 1 diabetes (and other forms of diabetes requiring insulin treatment) is managed in schools. Diabetes is not a static condition: blood sugars can change from minute to minute, so it is important that school personnel are educated, equipped and available to support students with diabetes. Staff involvement is essential to the short- and long-term health of students with diabetes, as well as to optimize their school performance.
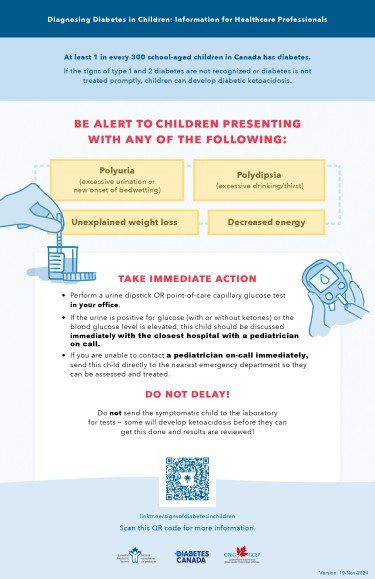
Children and youth spend about 30 to 35 hours per week in school – close to half of their waking hours – underscoring the importance of ensuring that students with diabetes are safe and well-managed. One in 300 children has diabetes, so it is very likely that most schools will have at least one student with diabetes at any given time. School personnel may be the first to notice symptoms of undiagnosed diabetes in a child (excess thirst, excess urination and weight loss). Prompt recognition of symptoms leading to early medical assessment can prevent diabetic ketoacidosis (DKA, see Appendix), a life-threatening complication.[1]
Support for students with diabetes is inconsistent across Canada. There are discrepancies in resources and policy across the country, even among schools in the same jurisdiction.
The goal of this statement is to ensure safe and fair treatment of students with diabetes through consistent and comprehensive provincial/territorial policy. These recommendations are directed to provincial governments – in particular policymakers in education and health departments – as well as to regional school boards, school administrators and teachers. This document is also a resource for children and youth with diabetes, and their parents or caregivers.
Background
The onset of type 1 diabetes is usually in the paediatric age range, making it one of the most common chronic diseases in children. In 2008–09, 3,287 new cases of diabetes (including both type 1 and type 2) were reported among Canadians aged one to 19 years, bringing the total number of cases in children and youth to 25,693. This represents a prevalence of 1 in 300 children.[2] In Canada, as in other parts of the world, the incidence is increasing steadily each year.[3]-[5] Children younger than five and early school-aged children are the fastest growing segment of the population with type 1 diabetes.[2][6]
Type 1 diabetes is associated with risk of complications in both the short term (hyperglycemia or high blood glucose, hypoglycemia or low blood glucose [see Appendix]) and long term (including heart attack, stroke, amputation, kidney failure, blindness, and learning deficits). Diabetes and its complications are a considerable burden on the Canadian economy.[7] Improved blood glucose control reduces both the onset and progression of diabetes-related complications in children and adolescents with T1D.[8]-[10] Therefore, optimal diabetes control is essential for individuals and society.
Diabetes and children
Diabetes management involves attention to diet, activity, frequent blood glucose monitoring and the administration of insulin. For children, blood glucose checks are recommended at least four times daily (before each meal and at bedtime), with more frequent checks being optimal for all and required for some. Some children use continuous glucose monitoring systems or CGMs (see Appendix), which automatically check the glucose every 5 minutes.
Control improves with more injections per day and is generally optimized using multiple daily injections (MDI) or an insulin pump. MDI involves giving a base dose of long-acting insulin plus injections of rapid-acting insulin with each meal or snack (4 to 6 injections per day). Insulin pump users wear a device that continually provides a basal dose of insulin, and the individual must give a bolus of insulin through this pump before eating. The amount of insulin is calculated based on blood glucose levels, the amount of carbohydrate in the meal or snack, and planned physical activity.
Physical activity is an important element of blood glucose control. Because it improves the efficiency of glucose uptake into muscle and other tissues, physical activity can cause hypoglycemia. Children with diabetes should be encouraged to be physically active and should participate in all regular school activities. However, food intake and blood glucose monitoring is even more important around activity. Parents need to know about scheduled changes in school activity routines to adjust the insulin dose and meal plan to avoid low or high blood glucose. Not eating a full meal or snack can also put children and teens at risk of hypoglycemia.
Over time, both high and low blood glucose levels have been shown to have negative effects on learning:[5][11]-[14]
- Low blood glucose can develop over a few minutes and can affect concentration, thought processing, and behaviour in the short term. If recognized early, most episodes of hypoglycemia can be readily treated with a fast-acting source of sugar. Once the hypoglycemia has been treated, it can take up to 45 minutes for its effects on intellectual functions to resolve.[15] When low blood glucose occurs at the time of an exam or test, students may need special accommodation to complete the exam or test.
- The general consensus is that the acute effects of high blood glucose occur only when hyperglycemia (BG >15 mmol/L) is persistent and accompanied by symptoms of illness (eg, fever or vomiting). Therefore, accommodations for hyperglycemia when taking exams, tests or quizzes should be similar to those for any other acute illness. However, there is also emerging evidence that hyperglycemia is associated with slowing of cognitive performance on tests, with increased errors and slower responses on basic mathematical and verbal tasks. The effects of hyperglycemia are highly individualized, affecting about 50% of people tested. As such, acute hyperglycemia is not a benign event for many people with diabetes.[16]
Diabetes and the law
Under the Canadian Charter of Rights and Freedoms, every citizen, including people with disabilities, has the right to equal protection and benefit without discrimination.[17] In March 2010, Canada’s Parliament ratified the United Nations Convention on the Rights of Persons with Disabilities. All provinces and territories are now bound by the convention which, among other rights, ensures that “effective individualized support measures are provided in environments that maximize academic and social development, consistent with the goal of full inclusion.”[18] Legally, schools must reasonably accommodate the special needs of children, including students with diabetes.
Consistent with the right to education, schools should also minimize barriers that prevent children from the fullest possible learning experience. The Canadian Diabetes Association has developed Guidelines for the Care of Students Living with Diabetes at School[19] but in most jurisdictions these recommendations have not been incorporated into policy. The level of support that a child or youth receives depends on where they live, the school they attend, and often their family’s advocacy efforts.[20] For instance, British Columbia recently established provincial standards mandating administration of insulin and glucagon by trained, unlicensed (ie, not regulated by a health professional college) school personnel.[21] Yet in many other Canadian schools, children have little or no support for blood glucose monitoring or other important diabetes management tasks. Children with diabetes may also be refused entry into daycare or after-school programs.[22]
Managing diabetes at school
Support for students with type 1 diabetes should be individualized, and should adhere to the guiding principle “only as special as necessary.” This inclusive principle fosters individual dignity, personal independence and diabetes self-management, appropriate to a student’s age and stage of development.
Hypoglycemia
Mild or moderate hypoglycemia requires immediate intervention to prevent severe hypoglycemia, which involves loss of consciousness or seizure. Preventing and treating hypoglycemia involve several elements:
- Regularly scheduled meals and snacks, and adequate time to consume them.
- Adjusting either food intake or insulin doses for increased physical activity. In most cases at school, this means an extra blood glucose check and/or extra snack before physical activity.
- A clean area for blood glucose checks, where hands can be cleaned, with a sharps container to safely discard glucose test strips and lancets.
- Supervising young children in ways that help them recognize, treat and prevent hypoglycemia.
- For all children, ready access to their emergency kit (with glucose meter, fast-acting sugar source, extra snacks, etc.).
- For older children or teens, accommodations for tests, quizzes or exams (eg, extra time), since hypoglycemia is likely to affect test performance even after appropriate treatment of an acute event.
When hypoglycemia is suspected or confirmed, the student cannot be left unattended until an episode has been appropriately managed and resolved.
Potential barriers to safe and effective management of hypoglycemia in schools include, but are not limited to:
- incomplete training of school personnel;
- unscheduled activity and inactivity;
- altered meal or snack times; and
- lack of rapid access to a glucose meter and emergency and treatment supplies.
Absenteeism
Having support at school is important for every child’s safety and inclusion. For families living with diabetes, school-based supports are also important to their mental health and well-being. Minimizing preventable absences from school is another priority for both children and parents. School absenteeism is not significantly higher in children with diabetes compared with other children, with the exception of absences for regular medical appointments.[23] Schools that use attendance-incentive programs may unintentionally punish or discriminate against students with diabetes. Any policy or practice that pressures students to forego medical appointments can negatively affect their well-being and unintentionally discourage them for taking responsibility for their health.
Facilitating safe diabetes care in schools and overcoming barriers
There are a number of potential barriers to optimal and safe diabetes management at school. Young children who are not independent in the daily tasks or decision-making around diabetes may not be able to benefit from MDI or insulin pumps when medically indicated, or their parents may have to leave the workforce to attend to their child’s diabetes needs at school. If support at school is limited, children may be started on only 2 to 3 insulin injections daily to avoid the need for a lunchtime injection.
Day-to-day care of students with diabetes does not require a medical professional at school. Every day, diabetes education teams teach and empower patients, families and caregivers to: monitor blood sugars; give insulin by injection or insulin pump; recognize and treat hypoglycemia; and supervise meals and snacks. Clearly, more intensive understanding and instruction is required to fully manage diabetes as a parent or caregiver, and this level of care cannot be expected of the school. Providing basic care to ensure safety and to perform standard diabetes management tasks while children are at school is rightfully expected and should be provided by trained school personnel. School employees should be aware that they will not be found liable if they take reasonable steps to assist a student with diabetes in an emergency situation.[19]
When a student has diabetes, it is important that the school be informed at two levels:
1. They require initial education and periodic updates about diabetes in children in general.
2. They need an individual care plan (ICP) specific to each student’s needs.
It is important to ensure consistency in the education provided to schools. With a new diagnosis of diabetes, families are often overwhelmed with information and are still adapting to a new reality. It may not be an appropriate time for them to educate school personnel. While diabetes educators have the knowledge and skills to provide this education, they typically do not have the time to educate individual schools. Regional or provincial health authorities must identify mechanisms to ensure that personnel and resources are made available to provide education to schools and that the education is specific to managing children with type 1 diabetes (eg, including online resources and community health nurses). Moving forward, it will be important to work towards common national resources.
Each year, schools should be provided with verbal and standardized written information about the child’s diabetes care requirements in school. Parents can complete information forms with or without the assistance of their diabetes team. In some circumstances, a virtual or in-person meeting between the child and parents, diabetes team and school personnel may help to clarify care requirements and roles. Some school boards employ a chronic disease liaison nurse and have found this role to be valuable in supporting diabetes management in schools. In many cases, parents are capable of providing information and resources without the need for a health care professional.
Recommendations
The Canadian Paediatric Society and the Canadian Pediatric Endocrine Group recommend that minimum standards for supervision and care be established across Canada to support children and youth with type 1 and other insulin-requiring diabetes in schools. The following recommendations are derived from evidence-based clinical practice guidelines,[11][24][25] with input from diabetes care providers from across Canada, and are consistent with the Canadian Diabetes Association’s Guidelines for the Care of Students Living with Diabetes at School.[19]
Provincial/territorial governments should establish comprehensive policies that include the following components:
- Schools having one or more students with diabetes must ensure that at least 2 school personnel are trained to provide support. Staff members may be unlicensed (ie, not regulated by a health-profession college), and will be provided with diabetes education resources and enabled to attend annual diabetes updates.
- Provinces/territories or regions should establish mechanisms to ensure adequate personnel and resources are available to provide diabetes education to schools, and that the education is specific to managing diabetes in children.
- Schools must provide all students with a clean, convenient and safe area for diabetes self-care, and respect students’ personal preference for privacy. Self-care tasks include blood glucose monitoring and the administration of insulin via injection or insulin pump. The level of autonomy will vary based on age and the individual child. The youngest children will need school personnel to provide all aspects of glucose monitoring and insulin administration, while older elementary school students are likely to need supervision only. As students mature, they are typically more able to provide self-care. School personnel should be identified and trained within the school to support students as needed.
- An individual care plan (ICP) must be developed for each student with diabetes and discussed among parents or guardians and the school principal (or designate) and teacher, with input from a health care provider as needed. The ICP should clearly outline roles and responsibilities of school personnel, parents and the child with diabetes. Discussions should occur before the start of the school year. Ideally, provincial authorities would make available a standardized form for this purpose.
- A designated staff member must supervise students’ meals and snacks to ensure that they are eaten on time and in full. Adequate time must be provided to consume the meal or snack. The level of supervision will vary based on the age and autonomy of the student.
- Each teacher or supervisor of a child with diabetes must know how to recognize and treat hypoglycemia. Regardless of age, a student must not be left alone when hypoglycemia is suspected. In the event of severe hypoglycemia, school personnel should call 911. Giving intramuscular glucagon is the optimal treatment for a severe hypoglycemic event, but may not be feasible for all schools. However, if the emergency response time is expected to be more than 20 minutes, it is strongly recommended that school personnel be trained to administer glucagon.
- Accommodations are recommended for examinations, tests and quizzes. Students with diabetes must be allowed to keep a diabetes emergency kit at their desk, including a blood glucose meter, hypoglycemia treatment, and snacks as required. In the event of a hypoglycemic event in the half hour preceding or at any time during an exam, a student should be granted an additional 30 to 60 minutes as needed to allow for cognitive recovery from hypoglycemia.
- Diabetes care tasks should be integrated into the student’s regular daily routine. To preserve the dignity of the student and to promote normal behavioural and social development, exclusion of any kind should be minimal and only in accordance with the student’s ICP.
- Students with diabetes may have more frequent medical appointments. Attendance-incentive policies and practices should not be applied to students when they need to attend medical appointments.
Appendix
Definitions
- Type 1 diabetes (T1D): A medical condition in which the pancreas is no longer able to make insulin, leading to abnormally high glucose (sugar) levels in the blood. If left untreated, it can be life-threatening. In the past, it was also known as juvenile diabetes or insulin-dependent diabetes.
- Hypoglycemia: An abnormally low blood sugar level. In children with diabetes this is a level less than 4 mmol/L.
- Hyperglycemia: An abnormally high blood sugar level. Although in children this is typically defined as above 10 mmol/L, symptoms are usually not seen until blood sugars are above 15 mmol/L.
- Blood glucose (BG) level: Amount of sugar found in the blood. This can be measured by applying a drop of blood on a strip. This strip is inserted in a small device (glucose meter) and gives a reading.
- Diabetic ketoacidosis (DKA): A serious complication of diabetes associated with high blood sugar, abdominal pain, nausea, vomiting and ketones (fruity-smelling breath). If left untreated, it can be life-threatening.
- Continuous glucose monitoring system (CGM): A device that has a small sensor inserted under the skin and provides glucose level readings every 5 minutes.
- Insulin pump: A device used to administer insulin continuously through a small tube inserted under the skin. The same device is also used to give the extra insulin needed with meals or to correct high blood glucose levels.
Resources
There are many excellent resources to help familiarize school personnel with diabetes management, including:
- Diabetes@School: Training resources for use by educators, school boards, and parents of children with diabetes. Topics include understanding blood sugars, food and insulin, physical activity and type 1 diabetes, and communication between home and school. The site also features a template Individual Care Plan, which details all aspects of a student’s diabetes care while at school. Developed by the Canadian Paediatric Society, the Canadian Diabetes Association and the Canadian Pediatric Endocrine Group.
- Canadian Diabetes Association. Guidelines for the Care of Students Living with Diabetes at School (September 2014): https://www.diabetes.ca/DiabetesCanadaWebsite/media/Learn-About-Diabetes/Your%20Rights/Diabetes_Canada_KWDIS_Guidelines-(ENG).pdf
- B.C. Children’s Hospital. Online module for educators, “Taking Care of Diabetes at School”: http://www.bcchildrens.ca/health-professionals/learning-development/resources/diabetes-at-school
- B.C. Ministry of Education. Forms, plans, posters and more: www.bced.gov.bc.ca/health/diabetes/
- B.C. Ministry of Children and Family Development, Nursing Support Services. Practice standards, forms, other resources: http://www.bcchildrens.ca/our-services/sunny-hill-health-centre/our-services/nursing-support
- International Diabetes Federation. The Kids and Diabetes in School (KiDS) program includes an information package in eight languages, suitable for downloading and printing, as well as an app. Each product has sections for parents of children with diabetes, parents in general, children, and teachers: www.idf.org/education/kids
- IWK Health Centre Pediatric Diabetes Team in Halifax. Online video training modules for teachers, three modules from 9 to 13 minutes each: www.iwk.nshealth.ca/page/video-diabetes-school
Acknowledgements
This statement has been reviewed by the Adolescent Health and Community Paediatrics Committees of the Canadian Paediatric Society and the membership of the Canadian Pediatric Endocrine Group.
References
- Vanelli M, Chiari G, Ghizzoni L, Costi G, Giacalone T, Chiarelli F. Effectiveness of a prevention program for diabetic ketoacidosis in children. An 8-year study in schools and private practices. Diabetes Care 1999;22(1):7-9.
- Public Health Agency of Canada, 2011. Diabetes in Canada: Facts and figures from a public health perspective; Chapter 5 – Diabetes in children and youth: www.phac-aspc.gc.ca/cd-mc/publications/diabetes-diabete/facts-figures-faits-chiffres-2011/chap5-eng.php (Accessed August 15, 2014).
- DiaMOND Project Group. Incidence and trends of childhood Type 1 diabetes worldwide 1990–1999. Diabetic Med 2006;23(8):857-66.
- Karvonen M, Viik-Kajander M, Moltchanova E, Libman I, LaPorte R, Tuomilehto J. Incidence of childhood type 1 diabetes worldwide. Diabetes Mondiale (DiaMond) Project Group. Diabetes Care 2000;23(10):1516-26.
- Daneman D. State of the world’s children with diabetes. Pediatric Diabetes 2009;10(2):120-6.
- Newhook LA, Penney S, Fiander J, Dowden J. Recent incidence of type 1 diabetes mellitus in children 0–14 years in Newfoundland and Labrador, Canada climbs to over 45/100,000: A retrospective time trend study. BMC Res Notes 2012;5:628.
- Canadian Diabetes Association, December 2009. Economic tsunami: The cost of diabetes in Canada. The prevalence and costs of diabetes: www.diabetes.ca/CDA/media/documents/publications-and-newsletters/advocacy-reports/economic-tsunami-cost-of-diabetes-in-canada-english.pdf (Accessed August 15, 2014).
- Asvold BO, Sand T, Hestad K, Bjørgaas MR. Cognitive function in type 1 diabetic adults with early exposure to severe hypoglycemia: A 16-year follow-up study. Diabetes Care 2010;33(9):1945-7.
- The Diabetes Control and Complications Trial Research Group. Effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329(14):977-86.
- The Diabetes Control and Complications Trial Research Group. Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J Pediatr 1994;125(2):177-88.
- Wherrett D, Huot C, Mitchell B, Pacaud D; Canadian Diabetes Association Clinical Practice Guidelines Expert Committee, 2013. Canadian Diabetes Association clinical practice guidelines: Type 1 diabetes in children and adolescents. http://guidelines.diabetes.ca/Browse/Chapter34 (Accessed August 15, 2014).
- Schoenle EJ, Schoenle D, Molinari L, Largo RH. Impaired intellectual development in children with Type I diabetes: Association with HbA(1c), age at diagnosis and sex. Diabetologia 2002;45(1):108-14.
- Ferguson SC, Blane A, Wardlaw J, et al. Influence of an early-onset age of type 1 diabetes on cerebral structure and cognitive function. Diabetes Care 2005;28(6):1431-7.
- Strudwick SK, Carne C, Gardiner J, Foster JK, Davis EA, Jones TW. Cognitive functioning in children with early onset type 1 diabetes and severe hypoglycemia. J Pediatr 2005;147(5):680-5.
- Blackman JD, Towle VL, Sturis J, Lewis GF, Spire JP, Polonsky KS. Hypoglycemic thresholds for cognitive dysfunction in IDDM. Diabetes 1992;41(3):392-9. (also Lindgren M, Eckert B, Stenberg G, Agardh CD. Restitution of neurophysiological functions, performance, and subjective symptoms after moderate insulin-induced hypoglycaemia in non-diabetic men. Diabet Med 1996;13[3]:218-25.)
- CoxDJ, Kovatchev BP, Gonder-Frederick LA, et al. Relationships between hyperglycemia and cognitive performance among adults with type 1 and type 2 diabetes. Diabetes Care 2005;28:71-7.
- Canadian Charter of Rights and Freedoms, Part I of the Constitution Act, 1982, being Schedule B to the Canada Act 1982 (U.K.), 1982, c. 11. http://laws-lois.justice.gc.ca/eng/const/page-15.html (Accessed September 20, 2014).
- United Nations General Assembly Resolution 61/106, The Convention on the Rights of Persons with Disabilities and its Optional Protocol (December 13, 2006). Article 24: Education (Accessed September 20, 2014).
- Canadian Diabetes Association. 2014. Guidelines for the Guidelines for the Care of Students Living with Diabetes at School: www.diabetes.ca/getmedia/173678f6-1a4a-4237-bd55-aa7ba469a602/guidelines-for-students-in-school.pdf.aspx (Accessed September 5, 2014).
- Yewchuk L, Morrison JP, Yewchuk S. Special feature: Unsafe at school; Advocating for children with type 1 diabetes. BCMJ 2012;54(5):232-7: www.bcmj.org/special-feature-unsafe-school-advocating-children-type-1-diabetes (Accessed September 9, 2014)
- British Columbia Ministries of Health, Education and Children and Family Development. Provincial Standards: Support students with type 1 diabetes in the school setting. June 2014: www.bced.gov.bc.ca/health/diabetes/diabetes_support_in_school_settings.pdf. (Accessed September 6, 2014)
- Nabors L, Lehmkuhl H, Christos N, Andreone TL. Children with diabetes: Perceptions of supports for self-management at school. JSchool Health 2003;73(6):216-21.
- Glaab LA, Brown R, Daneman D. School attendance in children with Type 1 diabetes. Diabet Med 2005;22(4):421-6.
- Silverstein J, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes: A statement of theAmerican Diabetes Association. Diabetes Care 2005;28:186-212.
- Sperling M (editor-in-chief). ISPAD Clinical Practice Consensus Guidelines 2014. Pediatric Diabetes 2014:15(Suppl 20):1-290. Accessed September 9, 2014.
Disclaimer: The recommendations in this position statement do not indicate an exclusive course of treatment or procedure to be followed. Variations, taking into account individual circumstances, may be appropriate. Internet addresses are current at time of publication.